Haglund's Bursitis
What Is Haglund’s Deformity?
Haglund’s deformity is a bony enlargement on the back of the heel. The soft tissue near the Achilles tendon becomes irritated when the bony enlargement rubs against shoes. This often leads to painful bursitis, which is an inflammation of the bursa (a fluid-filled sac between the tendon and bone).
Cause of Haglund's Deformity
Haglund’s deformity is often called “pump bump” because the rigid backs of pump-style shoes can create pressure that aggravates the enlargement when walking. In fact, any shoes with a rigid back, such as ice skates, men’s dress shoes or women’s pumps, can cause this irritation.
To some extent, heredity plays a role in Haglund’s deformity. Inherited foot structures that can make one prone to developing this condition include:
- A high-arched foot
- A tight Achilles tendon
- A tendency to walk on the outside of the heel.
Symptoms of Haglund's Deformity
Haglund’s deformity can occur in one or both feet. The symptoms include:
- A noticeable bump on the back of the heel
- Pain in the area where the Achilles tendon attaches to the heel
- Swelling in the back of the heel
- Redness near the inflamed tissue
Diagnosis of Haglund's Deformity
After evaluating the patient’s symptoms, the foot and ankle surgeon will examine the foot.
Further examination of the foot can be very important, particularly for subtle injuries which require a high index of suspicion.
In addition, x-rays will be ordered to help the surgeon evaluate the structure of the heel bone.
Treatment of Haglund's Deformity
Non-Surgical Treatment
Nonsurgical treatment of Haglund’s deformity is aimed at reducing the inflammation of the bursa. While these approaches can resolve the pain and inflammation, they will not shrink the bony protrusion. Nonsurgical treatment can include one or more of the following:
- Medication. Oral nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be recommended to reduce the pain and inflammation. Ice. To reduce swelling, apply an ice pack to the inflamed area, placing a thin towel between the ice and the skin. Use ice for 20 minutes and then wait at least 40 minutes before icing again.
- Exercises. Stretching exercises help relieve tension from the Achilles tendon. These exercises are especially important for the patient who has a tight heel cord.
- Heel lifts. Patients with high arches may find that heel lifts placed inside the shoe decrease the pressure on the heel.
- Heel pads. Pads placed inside the shoe cushion the heel and may help reduce irritation when walking.
- Shoe modification. Backless or soft backed shoes help avoid or minimize irritation.
- Physical therapy. Physical therapy modalities, such as ultrasound, can help to reduce inflammation.
- Orthotic devices. Custom arch supports control the motion in the foot.
- Immobilization. In some cases, casting may be necessary.
When Is Surgery Needed?
If nonsurgical treatment fails to provide adequate pain relief, surgery may be needed. The foot and ankle surgeon will determine the procedure that is best suited to your case. It is important to follow the surgeon’s instructions for postsurgical care.
Treatment of Haglund's Deformity
To help prevent a recurrence of Haglund’s deformity:
- wear appropriate shoes; avoid shoes with a rigid heel back
- use arch supports or orthotic devices
- perform stretching exercises to prevent the Achilles tendon from tightening
- avoid running on hard surfaces and running uphill
Treatment Process
Preparation for Surgery
- Provide a complete list of your medications so you can be advises which to stopped prior to surgery,
- Treat any tooth, gum, bladder or bowel problems before surgery to reduce the risk of infection
- Stop anti-inflammatory medications (NSAIDs) at least seven days before the procedure.
- Stop or cut down smoking to reduce your surgery risks and improve your recovery
- Consider losing weight (if overweight) before surgery
Day of Surgery
- Report any infections to me prior to surgery as the procedure cannot be performed until all infections have cleared up.
- Do not consume alcohol - 24 hours prior to treatment,
- Do not eat or drink anything, including water, for 6 hours before surgery
- Avoid vigorous physical activity or exercise 24 hours prior to surgery,
During Surgery
- Administration of general anesthesia or sedation and local anesthesia
- The entire procedure can take 60 minutes to two hours.
- Procedure is performed and sent to recovery room, for observation
- Pain medications are prescribed to help with pain during the recovery phase.
After Surgery
- Do not consume large amounts of alcohol after surgery,
- Avoid vigorous physical activity or exercise until advised,
- Follow the Post Surgery Treatment Plan proscribed by the surgeon and post op care specialists.
- Any questions or complications should be communicated directly to the surgeon
Common Questions
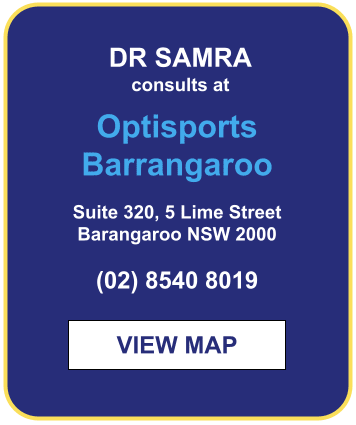
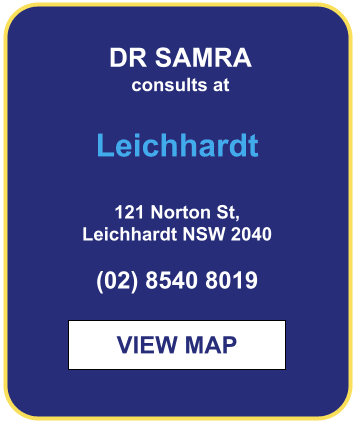
If you have a specific question about your treatment, we recommend contacting the clinic