Osteopenia & Sarcopenia
As we age, we tend to lose muscle and bone mass. These are important indicators of health and function. Sarcopenia is loss of muscle mass, while osteoporosis and osteopenia are different severities of loss of bone mass.
Dr Samra is a firm believer in Exercise is Medicine, and that all people should enjoy the health and longevity benefits of exercise, especially older patients.

The maintenance of muscle and bone mass is best achieved through maintenance of stimulus for muscle regeneration and adequate dietary substrate.
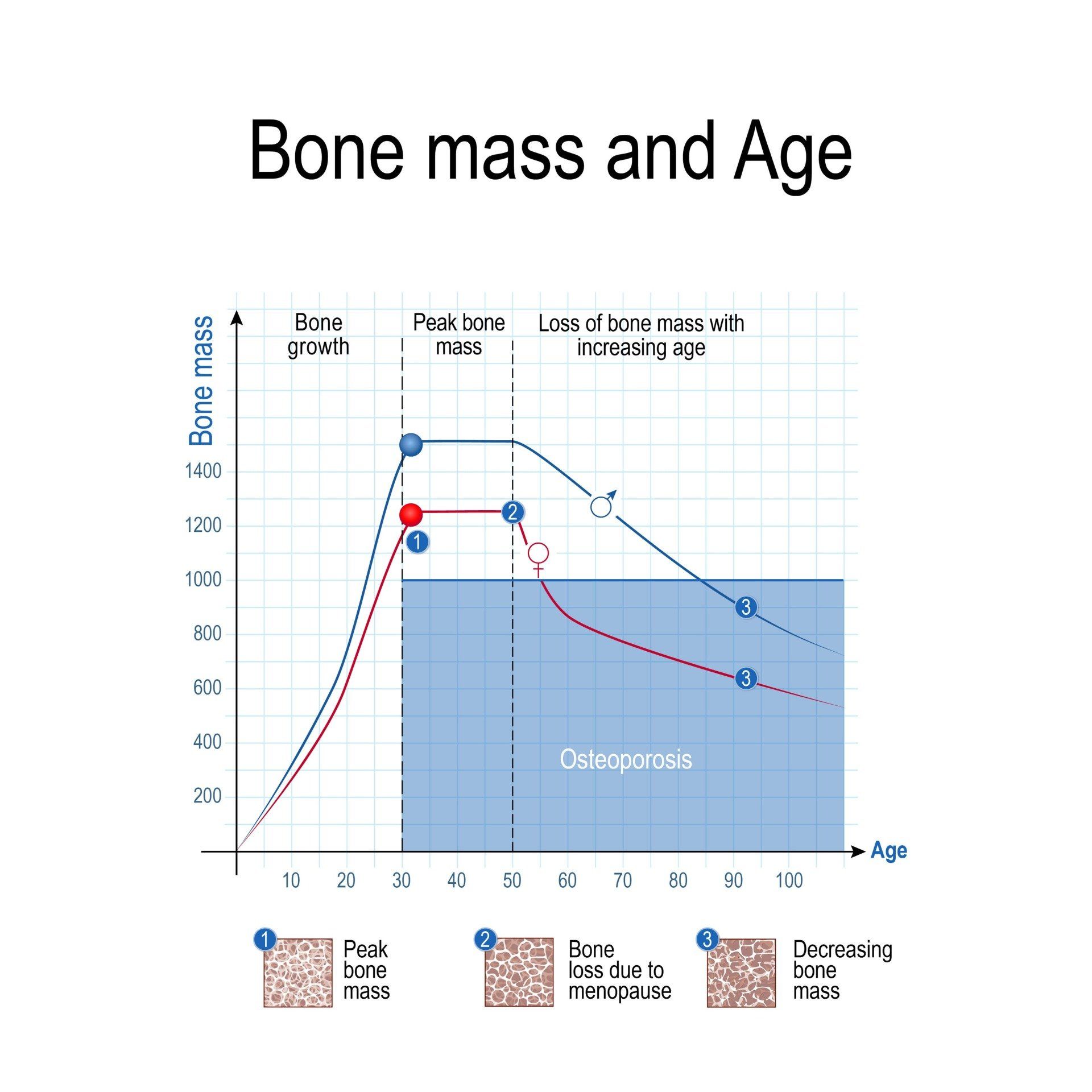
Osteoporosis is defined as a bone mineral density that is under 2.5 standard deviations below the average 30-year-old sex-matched person for height and ethnicity. Osteopenia is between 1 and 2.5 standard deviations below average. Low bone mass can be diagnosed in younger men and women when they are under 2 standard deviations from their aged-matched average bone mineral density. The lowest score of the hip and spine are taken to be the final score.
Unfortunately, it is very difficult to regain bone mass once it is lost. It tends to reach a peak in the mid-20s and then decline by about 1% per year (until after menopause in women where it declines by 2% per year). Patients with low bone mineral density are at risk of “fragility fractures” where minimal trauma breaks bones.
However, despite our best intentions we do not seem to do a very good job at preventing fragility fractures. Conventional medical treatments targeting osteoporosis and low bone mass tend to be “anti-resorptive” so that bone turnover is reduced overall.
Normally, there is a very intimate relationship between the cells that breakdown bone (osteoclasts) and the cells that build it up (osteoblasts). We call this “coupling”. These anti-resorptive drugs slow the breakdown of bone but they do not increase new bone formation.
While bone density appears to be preserved or improved in many patients, we are still not certain how much actual benefit they provide in terms of REDUCING FRACTURE RISK. Although many studies are industry funded, studies show that 20 women need to be treated with bisphosphonate drugs for 3 years to prevent one vertebral fracture, and 100 women need to be treated for 3 years to prevent one hip fracture (called the “Number needed to treat”).
While apparently quite safe, there have been concerns that these medications can actually increase fracture risk by changing the architectural stiffness of the bone, even if they help with the bone mass. There is reasonable evidence to support their use in high-risk cases and for secondary prevention (osteoporotic fracture/s have already occurred).
How are Osteopenia and Sarcopenia diagnosed?
Most patients are UNDIAGNOSED with both disorders.
Following a fracture caused by a minor fall or incident, this is when further investigations are often instigated to diagnosed low bone mass. A DEXA scan (Duel Energy X-Ray Absorptiometry) is a simple imaging technique that takes about 5-10 minutes and can assess both muscle AND bone tissue. More advanced techniques for assessing bone architecture include specialised volumetric CT scans.
Most patients with sarcopenia are never diagnosed. More attention is paid to patients with conditions that markedly increase the loss of muscle mass, such as cancer. It is now recognised that resistance and aerobic exercise improves symptoms and quality of life in patients who are actively undertaking cancer treatment, and Exercise Physiologists are now a very important part of cancer care. Lack of muscle leads to impairment of functional strength (weaker muscle) and metabolic health (less ability to dispose of glucose). Quality of life can be markedly improved through increases in functional muscle mass.
How are Sarcopenia and Osteopenia Treated?
This is where exercise and diet comes in.
Bone and muscle are both living, dynamic tissues that adaptively respond to the loads placed on them. While we may not be able to improve bone mass significantly, we can prevent fragility fractures by improving balance, muscle strength and the architecture of existing bones- all through the right kind of exercise.
Bone cells respond to peak forces in laying down new tissue, better than they do to repetitive forces. Interestingly, they are only responsive to these mechanical signals every 8 hours and then they become unresponsive to further stimulus within that 8-hour period. Therefore, periodic strength and impact exercises 2-3 times per day can be prescribed and supervised to maximise both muscle and bone strength.
If you feel that you are becoming frail, do not wait until it affects your life profoundly. Invest in your health and make exercise a part of your life. You will get out what you put in.